Parler
Parler Gab
Gab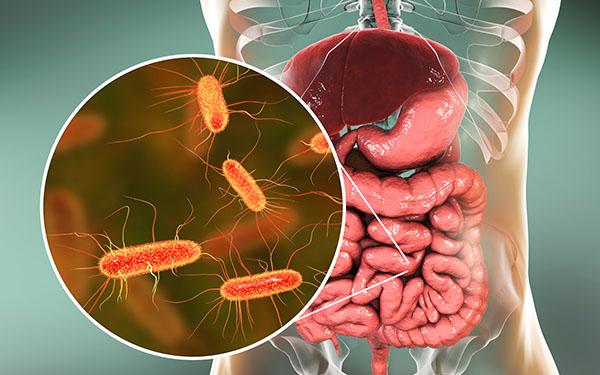
- Pharmaceuticals rewire your gut for years: 42% of drugs tested (including beta-blockers, antidepressants, and PPIs) altered the microbiome long after discontinuation, with some effects lasting over three years.
- The more drugs you take, the worse the damage: Cumulative prescription history compounds microbiome disruption, reducing bacterial diversity—a key marker of gut health.
- Benzodiazepines (like Xanax) are as destructive as antibiotics: These anxiety drugs decimate gut bacteria with effects rivaling broad-spectrum antibiotics, yet doctors prescribe them like candy.
- PPIs (heartburn meds) turn your gut into a Petri dish for oral bacteria: By suppressing stomach acid, they allow mouth bacteria to colonize the intestines, increasing infection risks.
- The study exposes a glaring blind spot in medicine: Researchers and doctors rarely account for past drug use when studying gut-related diseases, meaning millions of diagnoses may be wrong.
- Your microbiome may never fully recover from antibiotics: Even years after use, past antibiotic exposure was linked to permanently reduced bacterial diversity—a red flag for chronic illness.
- This is a corporate cover-up in plain sight: The FDA and CDC ignore long-term microbiome damage from drugs, while Pharma rakes in trillions from medications that sabotage your health.
- Natural alternatives aren’t just “woo”—they’re survival: With drugs acting like biological time bombs, detoxing, probiotics, and herbal medicine aren’t just preferences—they’re necessities.
How today’s pills become tomorrow’s gut disasters
For decades, the medical establishment has treated the human body like a mechanical problem—pop a pill, fix the symptom, move on. But what if the pill itself is rewiring your biology in ways that outlast the treatment? That’s exactly what this Estonian study reveals. Researchers didn’t just look at people currently taking medications; they tracked electronic health records over five years, comparing gut bacteria in those who’d taken drugs years prior to those who’d never taken them at all. The results were shocking. Take beta-blockers, for example—commonly prescribed for high blood pressure. These drugs don’t just lower your heart rate; they alter gut bacteria in ways detectable years after stopping. The same goes for proton pump inhibitors (PPIs), like omeprazole (Prilosec), which reduce stomach acid—a critical defense against pathogens. The study found that PPI users had higher levels of oral bacteria (like Streptococcus parasanguinis) in their guts, essentially turning their intestines into a microbiological free-for-all. When stomach acid is suppressed, bacteria that should stay in the mouth invade the gut, increasing risks of infections and inflammation. But the real bombshell? Benzodiazepines—Xanax, Valium, Ativan—were just as destructive to gut bacteria as antibiotics. These drugs, handed out like Skittles for anxiety and sleep disorders, wiped out microbial diversity with effects lasting years. Even worse, different benzos had different gut impacts—alprazolam (Xanax) was far more damaging than diazepam (Valium), yet doctors rarely consider this when writing prescriptions. And let’s not forget antidepressants, particularly SSRIs like Prozac and Zoloft. These drugs, which artificially alter serotonin levels, also reshape the gut microbiome—a cruel irony, given that 90% of serotonin is produced in the gut. So while Big Pharma profits from “treating” depression, the very drugs they push may be worsening the problem by destroying the gut-brain axis. So what happens when your gut microbiome is permanently altered by drugs? The consequences are far-reaching and devastating:- Immune system collapse: Your gut bacteria train your immune system. When diversity plummets, you become more susceptible to infections, allergies, and autoimmune diseases.
- Metabolic disaster: Gut bacteria regulate blood sugar and fat storage. Disrupt them, and you’re on a fast track to obesity, diabetes, and heart disease.
- Mental health sabotage: The gut-brain connection is real. A damaged microbiome is linked to depression, anxiety, and even neurodegenerative diseases like Alzheimer’s.
- Nutrient starvation: Your gut bacteria help digest food and absorb vitamins. Kill them off, and you starve your body no matter how “healthy” you eat. Increased cancer risk: A low-diversity microbiome is associated with higher rates of colorectal cancer, the third-leading cause of cancer deaths in the U.S.
Detox, rebuild, and reclaim your health
The human body is resilient, and the gut microbiome can heal—if given the right support. Here’s how to fight back: Detox like your life depends on it:- Probiotics: Look for diverse, soil-based strains (not just Lactobacillus).
- Prebiotics: Resistant starches (green bananas, cooked-and-cooled potatoes) feed good bacteria.
- Antimicrobial herbs: Oregano oil, garlic, and berberine can help rebalance gut flora.
- Fasting: Gives your gut a chance to reset.
- Bone broth and collagen: Heal the gut lining damaged by drugs.
- PPIs (Prilosec, Nexium): Try apple cider vinegar, digestive enzymes, or DGL licorice instead.
- Benzodiazepines (Xanax, Valium): Magnesium, L-theanine, and CBD can ease anxiety without gut destruction.
- SSRIs (Prozac, Zoloft): St. John’s Wort, 5-HTP, and therapy often work better long-term.
- Statins: CoQ10, red yeast rice, and niacin support heart health without gut harm.
- Fermented foods: Sauerkraut, kimchi, kefir—nature’s probiotics.
- Fiber-rich plants: Feed good bacteria (but avoid processed “fiber” additives).
- Polyphenol-rich foods: Berries, dark chocolate, green tea—these fuel beneficial microbes.
- Avoid seed oils and processed sugar: They feed harmful bacteria and fuel inflammation.
Federal appeals court permits Trump to DEPLOY National Guard to Portland
By Ramon Tomey // Share
Ayatollah Khamenei rebukes Trump’s claim that Washington destroyed Iran’s nuclear program
By Ramon Tomey // Share
EU moves to phase out Russian gas imports by 2028 amid Ukraine war fallout
By Belle Carter // Share
Violence and harassment target Syrian students in German schools
By Zoey Sky // Share
Study links ultra-processed plant-based meat alternatives to depression and inflammation
By Willow Tohi // Share
Governments continue to obscure COVID-19 vaccine data amid rising concerns over excess deaths
By patricklewis // Share
Tech giant Microsoft backs EXTINCTION with its support of carbon capture programs
By ramontomeydw // Share
Germany to resume arms exports to Israel despite repeated ceasefire violations
By isabelle // Share